Face & Neck Keloids
Keloid scars on the face and/or neck can be particularly distressing as they can be disfiguring, painful and can even get infected. Keloids on the face and neck are often the result of conditions such as recurrent cystic acne or ingrown hairs. They are less often the result of traumatic injuries or surgery. Depending upon the cause of the Keloid, treatment options vary.
At Rejuvence Clinic we offer a thorough and comprehensive range of treatment options for Keloid scars in people of all ethnicities. Many of our clients come to us with troublesome Keloid scars on the face and neck.
What are keloids?
Keloids or keloid scars develop as a result of an overgrowth of collagen within cuts or wounds. They can also occur after treatments such as aggressive lasers or deep chemical peels. Keloids are defined as raised scars that extend beyond the borders of the original cut or wound. They can grow to significant size and can often also be associated with itching and peeling. They can be very challenging to treat and are often associated with a significant rate of recurrence.
What causes keloids on the face and neck?
Keloid scars on the face and neck can be the result of medical conditions, injuries or surgery. There are also differences between men and women.
Who is prone to keloids on the face and neck?
Keloid scars are generally more common in those of Asian, Southeast Asian and Afro-Caribbean decent. There are a large number of causes of keloids on the face and neck. These can be the result of specific medical conditions or following surgery.
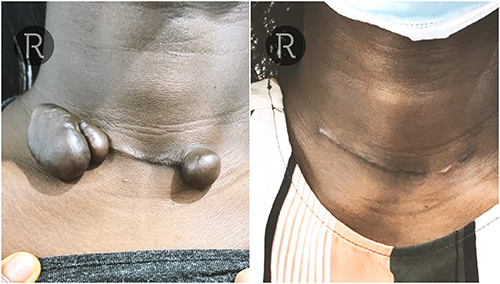
Before & Afters
©Individual results may vary.


























©Individual results may vary.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

©Individual results may vary.
Acne
In those susceptible to Keloid scarring, longstanding cystic acne associated with recurrent infections can result in the formation of large aggressive Keloid scars. These typically occur along the jaw line and on the cheeks in both men and women. They are usually the result of a vicious cycle of inflamed acne spots that fill with pus and subsequently ‘pop’ resulting in breaks in the skin that heal in the form of a keloid. As the cycle repeats itself the Keloid scars get further irritated and subsequently get larger.
Ingrown Hairs
When acne occurs in hair bearing regions of the face, the formation of acne Keloid scars can cause trapping of hairs – ingrown hairs. As these hairs attempt to grow below the skin the body reacts to them eliciting an inflammatory response essentially resulting in a type of folliculitis. This secondary infection or reaction can make Keloid scars even worse. This typically affects men in the beard region but can also affect women suffering from excess hair growth along the jaw line, chin and even the neck.

©Individual results may vary.
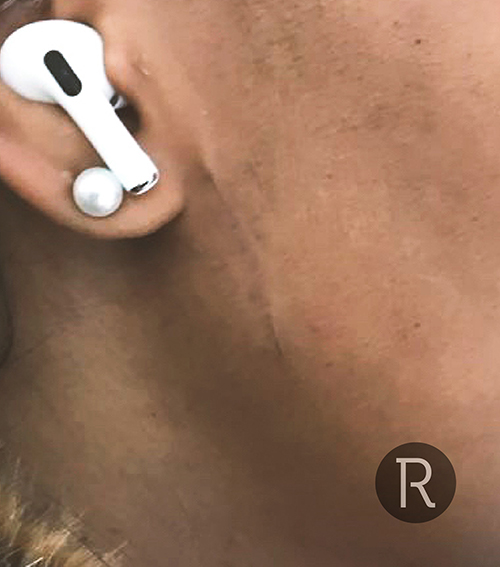
Shaving Bumps

©Individual results may vary.
Aggressive shaving, especially for those with very curly hair within the beard can also result in ingrown hairs. When these hairs start to grow under the skin they cause a ’foreign body’ reaction and result in what are typically known as ‘shaving bumps’. The medical term for this is folliculitis – inflammation of the hair follicle. This can be very itchy and irritating and repeated scratching, especially during the night, can cause breaks in the skin and this can subsequently heal in the form of a keloid.
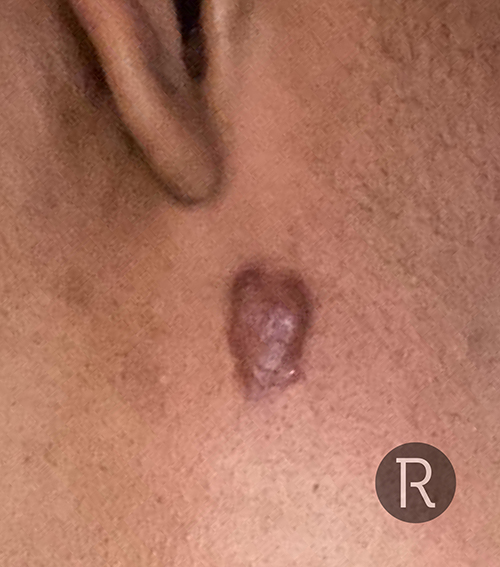
Surgery
Facial surgery resulting in long scars can eventually become keloid in nature. However, the risk of developing keloids on the face is generally quite low when considered with other parts of the body. Nevertheless this can still happen, hence long-standing regular dosing with steroid injections or 5-FU.
©Individual results may vary.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

©Individual results may vary.
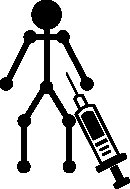
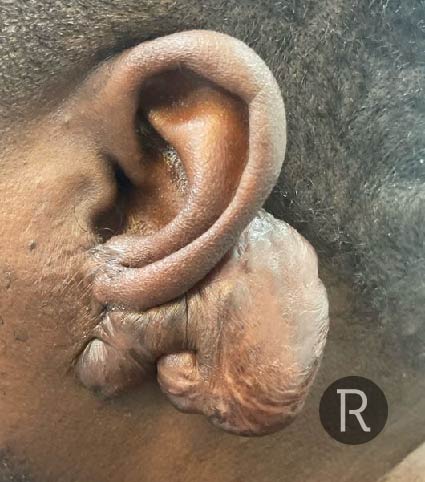
Piercings
As is the case with keloids on the ear, piercings, especially just in front of the ears (the pre-auricular region), can result in the formation of a keloid. These normally develop just in front of one or both ears and can extend into the ear.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.
What treatments are suitable for keloids on the face and neck?
The treatment of keloids in general is often challenging and a long term commitment. Rates of recurrence are relatively high and a preemptive approach is always much more effective than a reactive one. The specific locations of keloids pose different challenges and hence the same approach to treatment is not always appropriate. There are a number of treatment options for keloids on the face and neck and often the best approach is a combination rather than a single treatment.
Intralesional Steroid Injections
Injections of steroid into keloid scars is considered first line treatment. This applies to keloids occurring on the face and neck as well. Injections specifically into the body of the scar are known as intralesional injections and this approach limits complications typically associated with this treatment. The steroid helps to break down collagen scar tissue and also helps to prevent the keloid from growing further. Depending upon the size and number of keloid scars, more than one session of intralesional steroid injections may be needed.
Complications of intralesional steroid injections include skin atrophy (thinning of the skin) and hyperpigmentation (lightening of the colour of the skin). The incidence and severity of these complications are dependent upon the accuracy of the injections, the concentration of steroid used, the number of sessions, as well as the cause of the keloid scars in the first place. Ethnic background can also influence complication rates with hypopigmentation, being particularly troublesome in darker coloured ethnicities such as Afro-Caribbean and Southeast Asian. In contrast, skin atrophy is more of a problem in Caucasian and Middle Eastern skin types.
Intralesional chemotherapy injections
New research has demonstrated the effectiveness of intralesional chemotherapy injections for keloid scars, especially when they are combined with steroids. Chemotherapy injections help to breakdown, collagen scar tissue and have the added advantage of less skin, atrophy and hyperpigmentation as compared with steroids. However, chemotherapy injections are not able to Breakdown keloid scar tissue at the same rate as intralesional steroid injections when used as a standalone treatment. Chemotherapy injections are best used in combination with steroids for particularly aggressive and stubborn keloid scars on the face and the neck.
YAG Laser Treatment
Over the last five years, YAG laser has been found to be very effective for the treatment of hypertrophic and keloid scars. This particular laser is also used for hair removal in darker skin types and generally safe on all skin types. YAG laser helps to break down collagen scar tissue and also has a significant impact on helping to improve the colour of Keloid scars. When combined with intralesional, steroid and chemotherapy injections, excellent results can be achieved for keloids on the face and neck.
YAG laser has the added advantage of being very effective in the destruction of hair follicles and sebaceous glands. As discussed above, often keloid scars on the face and neck can be the result of cystic acne and ingrown hairs from shaving and waxing. By destroying the hair follicles, and sebaceous glands within a keloid scar, the incidence of new acne and/or ingrown hairs is reduced, and hence overall treatment is much more effective with better cosmetic results as well as a lower chance of recurrence.

Cryotherapy
Cryotherapy can be used to treat smaller, keloid, scars, resulting from acute flareups of folliculitis. They are particularly effective on the neck, especially for shaving bumps. Again, when combined with intralesional steroid injections, treatments goals can be achieved much faster. For larger keloids, cryotherapy can be slow and painful with a long downtime. They can also result in post-inflammatory hyperpigmentation. In our opinion, cryotherapy would be very much a third or fourth choice for treatment of keloid scars on the face and neck.
Surgery
The traditional view of surgery for keloid scars is that it is almost always associated with recurrence and keloids can grow larger than they originally were. Although there is some truth to this statement, surgery can often be very appropriate in certain cases, especially where the keloids are extremely large and causing significant psychological distress, as well as physical symptoms of pain and reduced range of movement. Surgery should always be offered in conjunction with further pre-emptive treatments to try to prevent keloid recurrence, for example, intralesional, steroid injections, and YAG laser post-operatively.

©Individual results may vary.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.
Rejuvence Approach
At Rejuvence, we have a wealth of experience in using a variety of treatment modalities to reduce and remove keloid scars on the face and neck. Following an initial assessment, we put together a management plan for all of our clients and this usually involves a combination approach as opposed to a single treatment. This is because combination treatments have been shown to be far more effective with better cosmetic results as well as being longer lasting. We can combine intralesional steroid injections, chemotherapy injections, surgery, and YAG, laser in a variety of combinations, depending on the location, size and cause of a keloid. Most importantly, it is essential to try to complete treatment and not end it prematurely when improvements are especially rapid. This will help to further prevent quick recurrence of symptoms.
Easy to contact us
Keloid scar treatments are often associated with a significant risk of recurrence. Failings of treatment received under the NHS has often been due to lack of access to prompt interventions whenever there is a flareup such as intralesional steroid injections or laser treatment. At Rejuvence Clinic, we ensure all of our clients can contact us easily via WhatsApp or phone to inform us immediately of any minor flare ups so that we can arrange urgent reviews in clinic with our doctors, and if need be, prompt intralesional steroid injections to control recurrence.
Hypopigmentation, following intralesional steroid injections, is usually the result of reduced melanin production associated with leakage of steroid medication into the local lymphatic vascular supply. Hence some areas of the body (for example, the shoulder and back) are more susceptible to hyperpigmentation than others. Melanin is responsible for our skin tone. The more melanin we have the darker skin tone. When melanin production is blocked, skintone returns to its default colour, which is very “white”. This is especially noticeable on darker skin types, whereas on lighter skin types, it is better camouflaged.
Generally complications from intralesional steroid injections, and to a lesser extent, intralesional, chemotherapy injections, are temporary and normally reverse over a period of many months. Reversal of hypo, pigmentation and skin atrophy usually occurs alongside recurrence of the keloid scar.
Skin atrophy associated with intralesional steroid injections can be quite tricky to improve. Skin atrophy is slightly more common in lighter skin types, especially Caucasian and Mediterranean patients as opposed to darker skin tones, originating from Africa and the Caribbean. When skin atrophy occurs, it can present in the form of “pitting” or “dips” in the skin. This usually tends to occur as a delayed effect of steroid treatment between 2 to 4 months afterwards. This is usually the result of residual steroid crystals that form a few weeks after the initial intralesional injection. The higher the concentration of steroid used the greater the risk of skin atrophy occurring.
This can be treated with a combination of normal saline sub dermal washouts followed by the use of specific PLLA filler to help restore the contour and encourage new collagen formation.
As mentioned above, depending on the location and size of the keloid, multiple intralesional steroid injection sessions may be required in order to achieve the best cosmetic result. Intralesional steroid injections can be performed up to 4 weeks apart. At Rejuvence, we often advisor client to go for a combination of YAG, laser and steroid injections
The main complication associated with YAG laser for the treatment of keloid scars on the face and neck is the risk of burns. YAG laser is considered a non-ablative laser as opposed to ablative. This means that it does not result in thermal damage to the top layer of the skin in the same way that is achieved by a CO2 Fraxel laser. Instead, it targets the deep, dermal layers of the skin, resulting in changes to the excess collagen scar tissue within a keloid. However, in certain specific types of keloid, for example, after a piercing, it can result in burns, especially when combined with intralesional steroid injections at the same sitting. At Rejuvence, we have a very conservative approach with a very low complication rate, associated with YAG laser treatment for keloid and hypertrophic scars.
With the focus of the YAG laser treatment being an improvement in the colour of Keloid scars, you often find that a large number of standalone laser sessions are required when compared with intralesional steroid or chemotherapy injections.
At Rejuvence Clinic we have had many patients attend informing us that their dermatologists have started them on oral retinoid tablets. These medications can only be prescribed by dermatologists and are often used for the treatment of severe acne affecting the face and back. They also require careful monitoring with regular blood tests. For regular facial and back acne oral retinoid treatment can be fantastic. However, whilst taking oral retinoid treatment, no dermatological or aesthetic treatments – non-surgical and surgical – can be carried out. This is due to this medication resulting in impaired healing. It has been found that patients suffering with keloids due to acne can have a flare up of their keloids with accelerated growth in size whilst on oral retinoid treatment. We do advise all clients suffering with keloids caution when considering oral retinoid treatment. In addition anyone on oral retinoids cannot have any treatments for at least 6 months after they have stopped this medication.