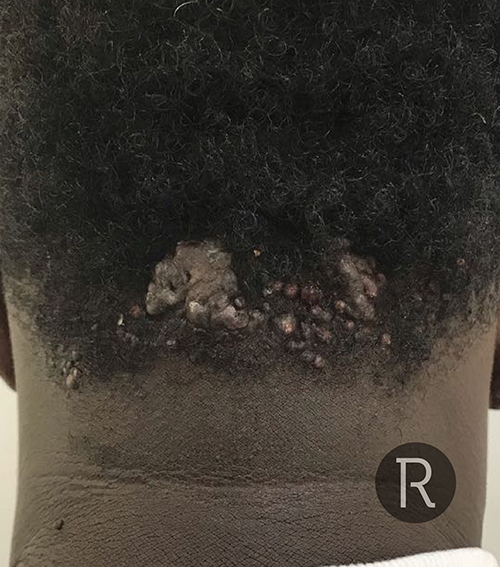
Scalp Keloids & Shaving Bumps
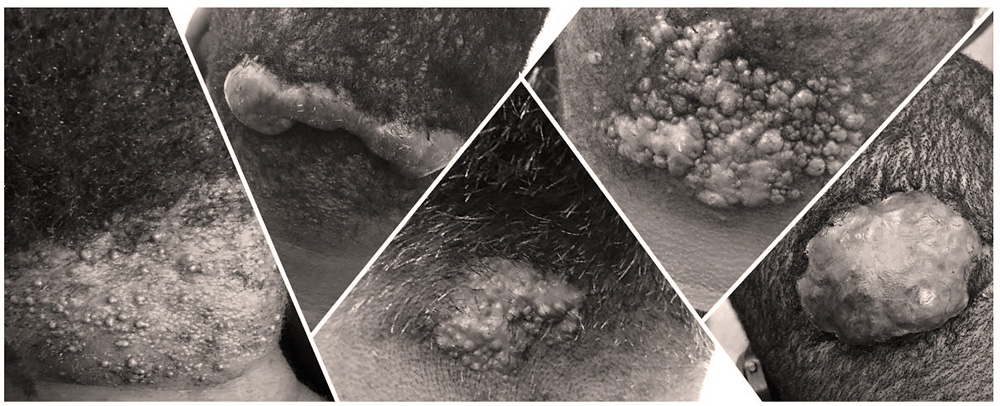
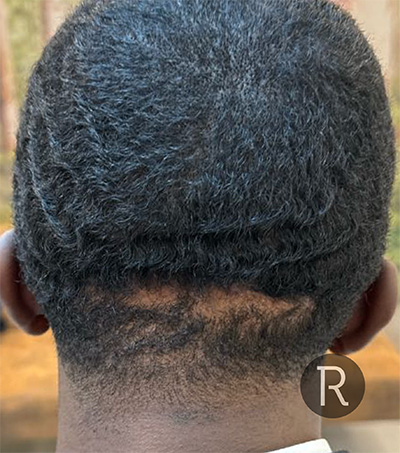
Shaving bumps on the back of the scalp, especially following a skin fade, are now quite common. These can be itchy, painful and get infected. In worst case scenarios they can progress to keloids. These keloids can continue to get bigger and bigger to the extent that many are left with distressing large, painful and inflamed lumps on the back of the head. This condition is known as Acne Keloidalis Nuchae. Keloid scars on the scalp can also be the result of surgery or trauma.
At Rejuvence Clinic we offer a thorough and comprehensive range of treatment options for Keloid scars in people of all ethnicities on the scalp. These keloids require a flexible approach to treatment to achieve the best results.
What are keloids?
Keloids or keloid scars develop as a result of an overgrowth of collagen following cuts from infected skin breaks associated with shaving bumps (folliculitis). They can also occur after surgery for lumps and bumps on the scalp or stitching of cuts following accidents or assaults.
Keloids are defined as raised scars that extend beyond the borders of the original cut or wound. They can grow to significant size and on the scalp, often get infected if there are trapped hairs within. They can be very challenging to treat and are often associated with a significant rate of recurrence.
Who is prone to keloids on the scalp?
Specific ethnic groups have an increased risk of developing keloid scars. Certain regions on the body are more prone to developing keloid scars irrespective of ethnic background. In the case of specific medical conditions, such as Acne Keloidalis Nuchae, Afro-Caribbean and Asian ethnicities are much more prone to developing this condition and subsequently keloid scars. Traumatic cuts to the scalp and/or surgery often results in hypertrophic and keloid scars in darker skin types.
What causes keloids on the scalp?
Keloid scars on the scalp can be the result of a medical condition, surgery or trauma.
Acne Keloidalis Nuchae
This condition is not very well-known and can result in a range of different types of keloid scars, including small papules (hard shaving bumps) to very large masses. Acne Keloidalis Nuchae starts with the formation of folliculitis following a skin fade haircut to the back of the scalp, and at the base of the neck. By shaving very close to the skin in these areas, in specific ethnic groups, especially Afro-Caribbean and Asian ethnicities, the cut hairs can grow inwards into or below the skin, resulting in ingrown hairs. These ingrown hairs set off what is known as a “foreign body reaction” and the subsequent inflammation results in the formation of shaving bumps also known as folliculitis.

Often those suffering with this type of folliculitis complain of severe itching and pain. They will often find their pillow bloodstained when they wake up in the morning from the constant itching during their sleep. Folliculitis can be complicated by infection and subsequent cuts to the skin from constant itching. They will eventually heal, but in the form of a keloid. If this process continues the keloids grow further, and can eventually go from small sparsely spaced papules that join together and form large, keloid tumours. Repeated shaving of the area, chronic infection, and persistent, ingrown hairs, all combine in a vicious circle, only making the keloid worse.
Surgery & Traumatic Cuts
Irrespective of ethnic background, the scalp can be prone to keloid formation more so than many other parts of the body. Therefore, scars, resulting from surgery for lumps and bumps, such as lipomas or sebaceous cysts, can often result in a hypertrophic scar that can progress to a keloid scar. In addition, traumatic injuries to the scalp, following accidents or assault can also result in keloid formation, especially if they are not given appropriate first aid treatment. Post operative and trauma related keloids tend to be more responsive to 1st line keloid treatments as opposed to keloids associated with acne Keloidalis Nuchae.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.
What treatment options are available for scalp keloids?
Keloids on the back of the scalp can be quite difficult to treat. They have a relatively high recurrence rate and often can be complicated by infection. Hence a flexible and responsive approach to treatment is required. There are a number of treatment options available and their use is dependent upon the nature and grade of the keloid scar.
Acne Keloidalis Nuchae
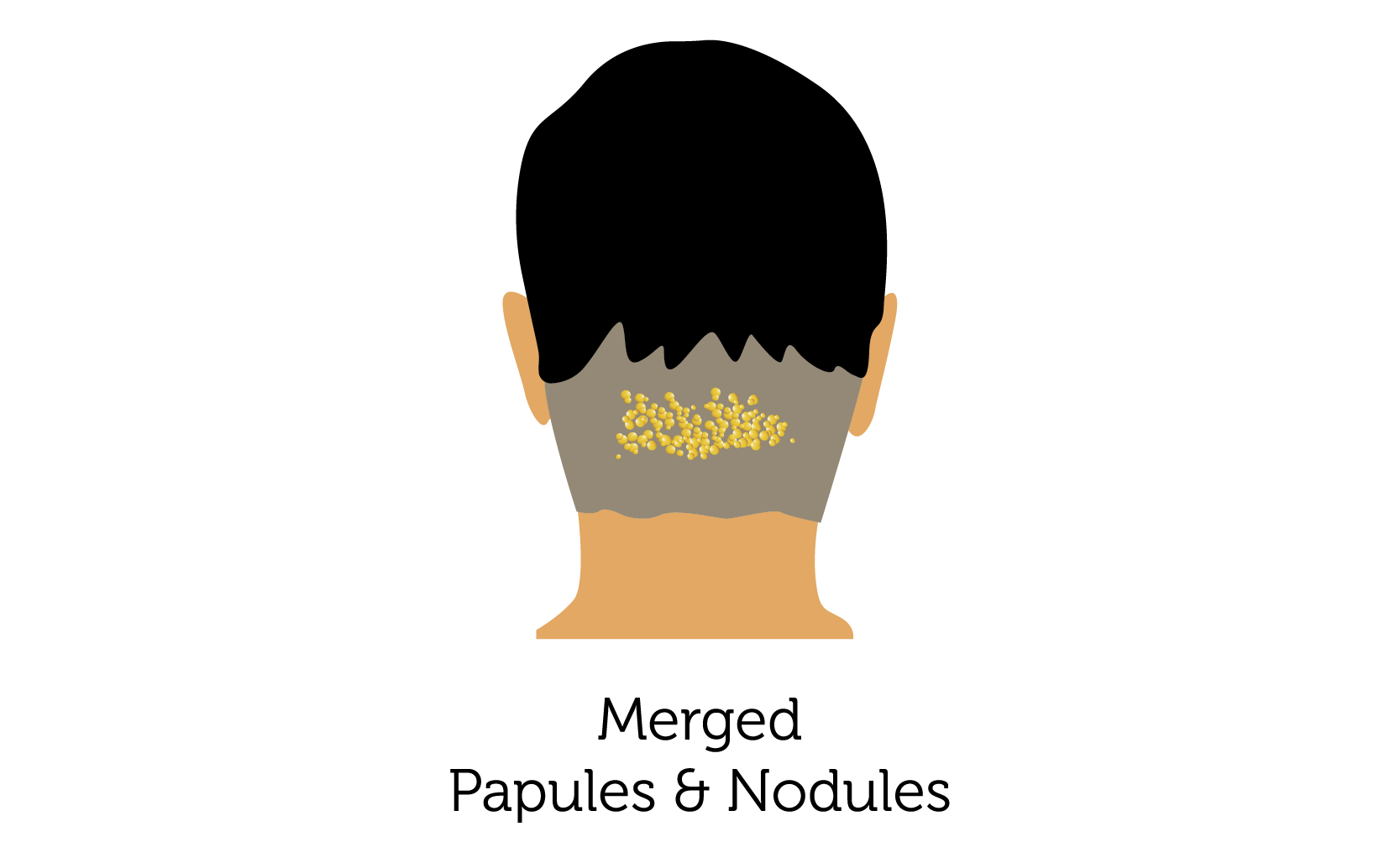
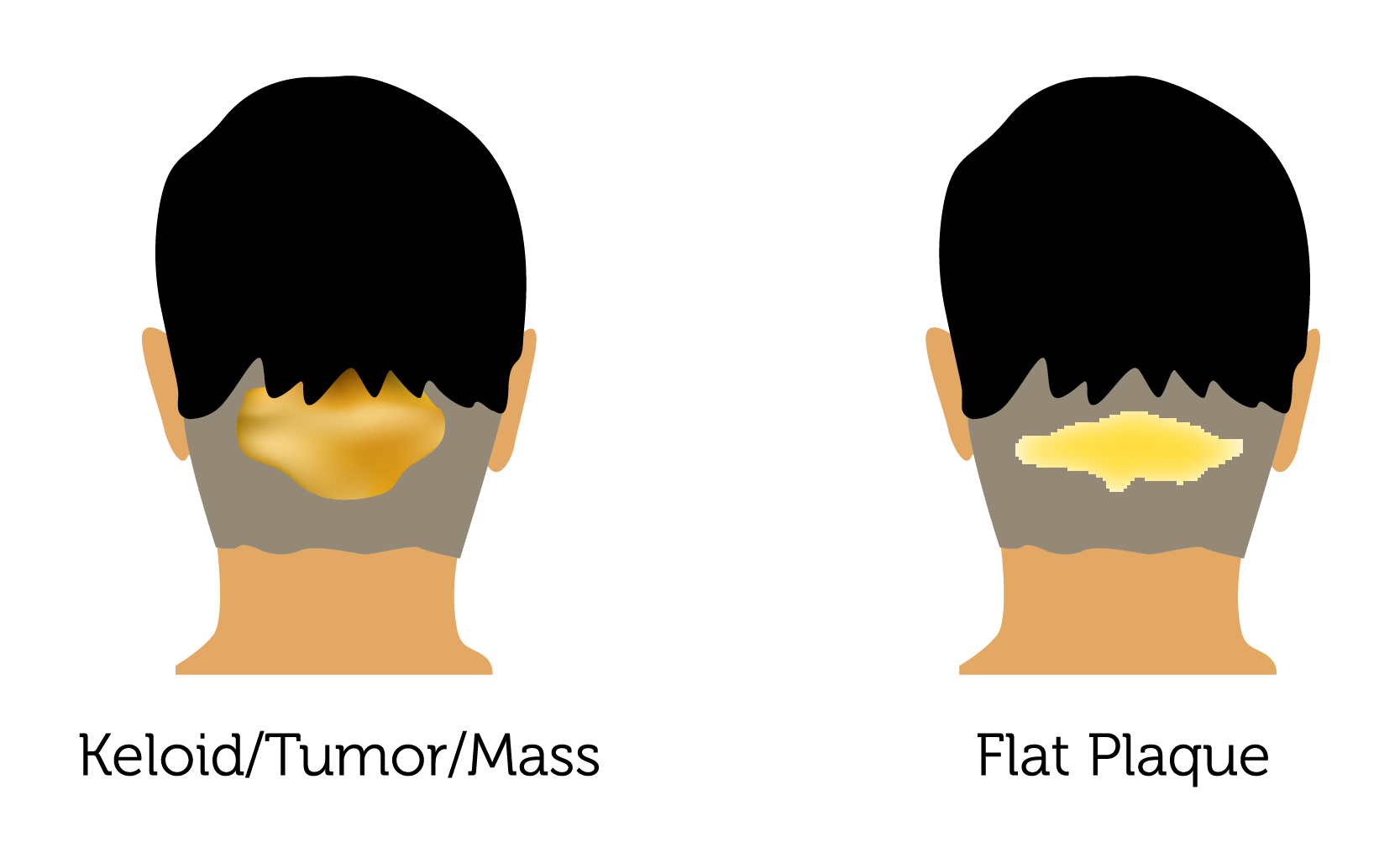
Acne Keloidalis Nuchae can be categorised into 4 grades of disease: (1) Papules; (2) Nodules; (3) Merged Papules & Nodules; (4) Keloid Tumour and (5) Keloid Plaque. Treatment options depend on the grade of the condition and the presence of any superimposed infection.
Papules & Nodules
Papules and nodules are the lowest grade of acne keloidalis nuchae. All keloids resulting from this condition initially start off as papules commonly known as ‘shaving bumps’. They will occur soon after having a skin fade at the back of the scalp and are the result of ingrown hairs. This can trigger irritation and itching and can be complicated by infection. Persistent itching can result in breaks in the skin, and can heal as small raised keloids, also known as papules. If these get reinfected, especially after repeated skin fades in the same area, they often get reinfected and the Keloid papules can grow to form larger nodules.
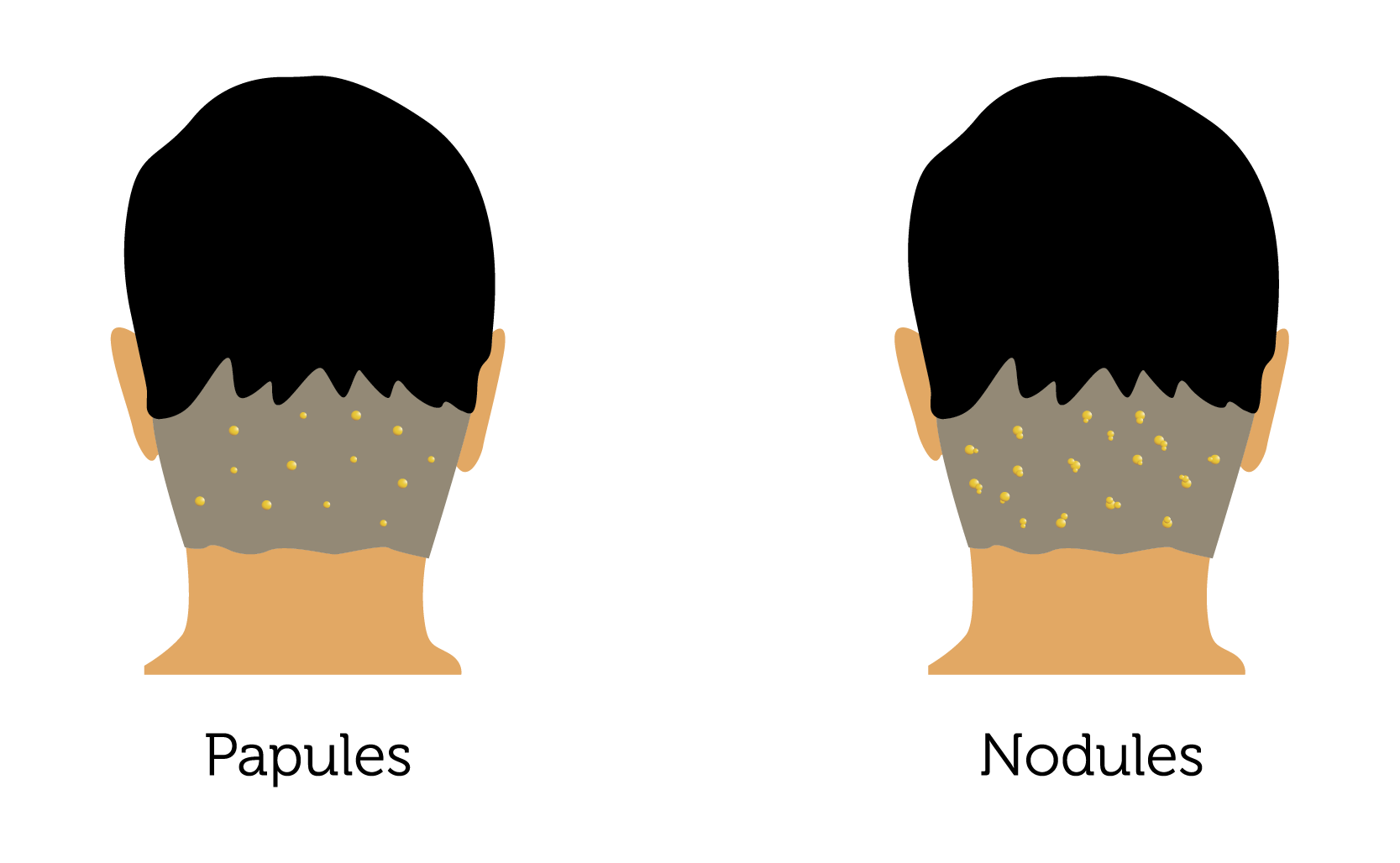
Treatment Options
- Stop getting skin fades: Before considering any sort of treatment, it is extremely important to understand you need to stop shaving the back of the scalp. Hair should only be cut using clippers and kept to a grade 1.5 or more otherwise the condition will continue to worsen due to repeated irritation.
- Antibiotics: Long-term preventative antibiotics (prophylactic) can help to fight off any persistent and chronic infection. This can help significantly reduce any irritation and itching. Antibiotics are also very helpful for improving the effectiveness of other more definitive Keloid treatments. The antibiotics however, will not on their own help reduce the already established keloid papules and nodules.
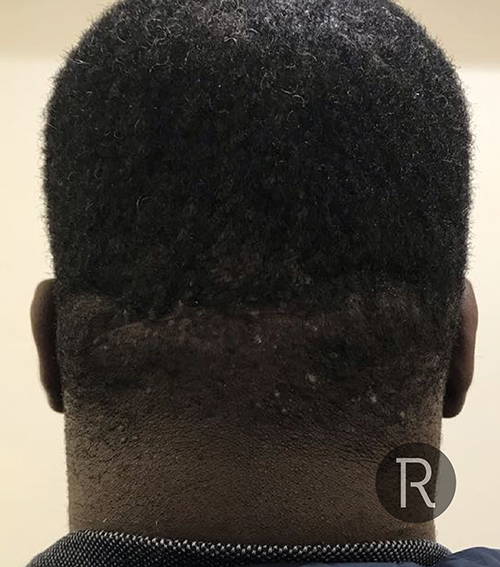
- Intralesional Steroid Injections: Keloid papules and nodules can be treated effectively with intralesional steroid injections. Steroid injections are considered first line treatment for Keloid scars. Nodules respond better to steroids than papules as they are slightly larger and hence easier to inject. The presence of infection and pus can make it difficult to get a good result with just intralesional steroids and hence we always recommend antibiotics as well. A course of steroid injections can effectively flatten many of the nodules and papules in milder forms of Acne Keloidalis Nuchae and offer excellent results.
- Aerolase Neo Elite (Nd:YAG): Recent research has found that YAG Laser treatment can be a game changer when it comes to the treatment of most grades of Acne Keloidalis Nuchae. Multiple sessions of YAG laser can reduce the size of the Keloid papules and nodules and is especially effective in combination with intralesional steroid injections. YAG Laser also helps to improve the colour of the papules and nodules. Most importantly the YAG laser will help to destroy the hair follicles trapped within the papules and nodules and eliminate the ingrown hairs. This significantly reduces recurrence rates and associated infection. At Rejuvence we use the Aerolase Neo Elite with other treatments and in some cases it can be the sole treatment for Acne Keloidalis Nuchae. Neo is a 650-microsecond pulse duration Nd:YAG laser. This means it can safely and effectively deliver higher energy levels to skin of colour without the need for cooling and minimal pain. Multiple studies have shown that 92% of patients of colour would recommend Neo Elite to others and 84% of patients reported no side effects. Patients reported a 75% reduction in papules associated with in-grown hairs (also known as pseudofolliculitis barbae) with Aerolase Neo Elite after 8 sessions.
- Cryotherapy & Ablative Aerolase Era Elite: Following initial treatment with a combination of YAG laser and intralesional steroid injections cryotherapy can be very effective for smaller papules as opposed to nodules. Freezing the small ‘shaving bumps’ can help to completely remove them and improve cosmetic appearance. The Aerolase Era Elite is our goto fully ablative laser that can carry out resurfacing safely and effectively in skin colour. Once papules have been shrunk, the remaining lesions can be ablated with Era to give an even better result safely in skin of colour.
Merged papules & nodules
If the condition is allowed to continue the papules and nodules can increase in number and start to merge, creating much larger keloid scars. An increase in trapped hairs also occurs and increases the incidence of infection that makes the papules and nodules very itchy and sometimes painful. A vicious cycle of infection and reinfection along side expanding Keloid makes the condition worse.
- Antibiotics: As with lower grades of acne Keloidalis Nuchae mid to long term low dose antibiotics can help to reduce inflammation. This in turn helps to control the rate of Keloid growth and provides a window of opportunity for further treatment.
- Intralesional steroid injections combined with Aerolase Neo Elite Nd:YAG Laser: Acne Keloidalis Nuchae results in the formation of keloids at the back of the scalp due to a combination of recurrent ingrown hairs, getting infected, resulting in skin breaks that eventually heal as keloids. As a result, for effective treatment, a combination approach is required to address this combination of symptoms. For merged papules, and nodules YAG laser helps to destroy trapped, ingrown hair, follicles within the keloid mass whilst intralesional steroid injections help to breakdown the keloid scar tissue itself. Although alone both treatments can be effective and improve symptoms ultimately, a combination approach helps, not only with reducing keloid size, but also reducing the frequency of future flare ups. In most cases, we find that at least 2 to 3 sessions of steroid and laser combination are required, followed by a further three sessions of standalone laser treatment are effective. At Rejuvence we use the highly acclaimed Aerolase Neo Elite 650-microsecond Nd:YAG laser for the treatment of acne keloidalis nuchae.
- Intralesional chemotherapy: In the case of stubborn, keloid scars, that, despite the combination approach of laser and steroid are not progressing quickly, intralesional chemotherapy injections in the form of 5-FU (5 Fluorouracil) can help to augment the effect of treatment. At Rejuvence, we aim to offer flexible treatment solutions and where we anticipate difficult keloids we will suggest adding in 5-FU injections alongside both steroid and laser treatment.
- Surgery: There is a common assumption that any surgical solution for keloid scars, irrespective of where they occur on the body will result in a high rate of recurrence with keloids returning often larger than they were before. This is not quite true, and is usually the result of no follow-up treatments being administered after surgery, such as steroid injections or laser treatment. There is no doubt that surgery is on its own will probably result in recurrence and even a poor outcome in the future. One criticism of surgical treatment provided on the NHS is that patients have found that there has been significant difficulties in access to follow-up treatment specifically steroids. This would also be complicated by the fact that the surgery would often be provided by plastic surgeon, but the steroid injections by dermatologist and due to poor communication They would be in adequate follow-up. As a result we see a lot of patients in our clinic they have had surgical interventions under the NHS and although a good cosmetic result initially have had significant recurrence. Any surgical solutions we offer at Rejuvence Clinic are part of a package of treatments including follow-up with steroid injections and laser treatment. In the case of merged, papules and nodules that are restricted to a small region, surgery maybe an option. However, our general approach is that in most cases, the individual sizes of the keloid papules, and nodules mean that they should be relatively responsive to nonsurgical treatments, such as steroid and laser combinations. In addition, the post-operative recovery time with surgery is quite long whereas downtime associated with non-surgical treatment methods is much shorter.
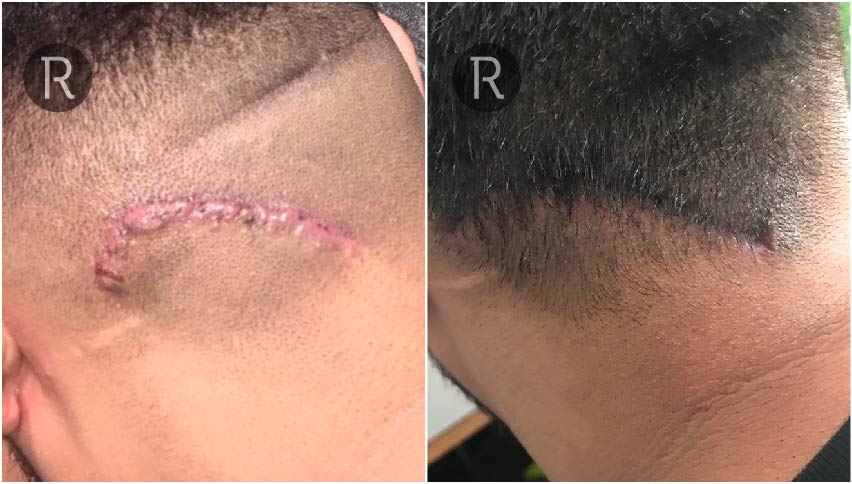
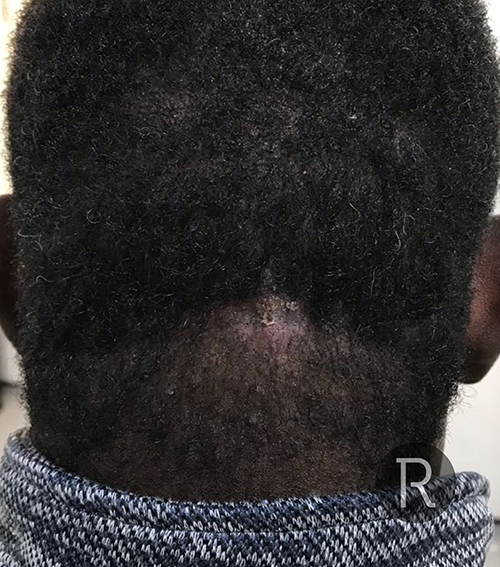
Before & Afters: Laser & Steroid










©Individual results may vary.
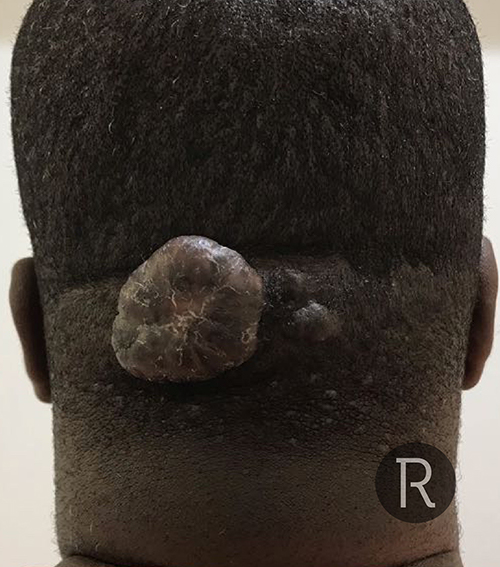
Keloid Tumours & Plaques
If Acne Keloidalis Nuchae continues to progress the merged papules and nodules, start to form an expanding keloid ‘tumour’ or mass. This can start to grow outwards away from the scalp presenting as a large lump on the back of the head or indeed, expand sideways and present as a sheet or ‘plaque’ of thickened fibrotic scar tissue across the back of the neck. This can be associated with significant pain and recurrent infection with pockets of pus filled abscesses within the tumour mass or plaque.
- Antibiotics and Aspiration: The larger the keloid becomes the more important it is to start and adhere to mid to long-term antibiotics treatment. The ingrown hairs that were responsible for originally triggering this condition will still be present within this tumour or plaque and hence will continue to exacerbate the condition. It is extremely important therefore to combat this recurrent infection with antibiotics. In cases of severe flare ups where pus has started to discharge from the keloid alongside the formation of abscesses, a short course of stronger antibiotics alongside incision and drainage of abscesses may be necessary.
- Surgery: In the case of large keloid tumours, conventional treatment options that may be first line for lesser grades of acne keloidalis nuchae are often not an option. Where we believe it will be possible to operate we do advise surgery for the removal of large keloid tumours. The excision is normally carried out under local anaesthetic. The associated downtime can be a little bit lengthy, in the range of 2 to 3 weeks. Thereafter, we would follow surgery up with a series of intralesional steroid injections to help prevent further keloid formation along the surgical scar. We also recommend antibiotics as a long-term measure, and may even advise YAG laser for ingrown hairs that may potentially trigger future recurrence.
- Scalp Micro Pigmentation: Following successful surgical excision of a keloid tumour and follow-up treatments, including intralesional steroid injections and YAG laser, it may be possible to consider camouflaging the scar to optimise the cosmetic outcome once treatment is considered to be complete. Scalp micro pigmentation is a treatment that can be used to colour the scar on the back of the scalp following surgery such that it is less visible. However, it is important to note that once SMP has been carried out YAG Laser treatment can no longer be carried out.
- Aerolase Neo Elite Nd:YAG Laser, Intralesional Steroid & 5-FU Injections: With further progression of disease, keloid tumours develop into keloid plaques. A plaque is a flattened hardened sheet of keloid where infection has resolved, but the scar has widened and is well set on the back of the scalp. At this point, plaques can be very hard to surgically remove simply because they are too large. Hence nonsurgical treatments are necessary to try to reduce it in size and prevent any further worsening of symptoms. A combination of Aerolase Neo Elite Nd:YAG laser and intralesional Steroid injections can be helpful. In more severe cases, it may be necessary to also administer intralesional chemotherapy injections, specifically 5-FU. As with all other grades of Acne Keloidalis Nuchae, long term preventative antibiotics should be taken.
©Individual results may vary.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.
Before & Afters: Surgical Excisions

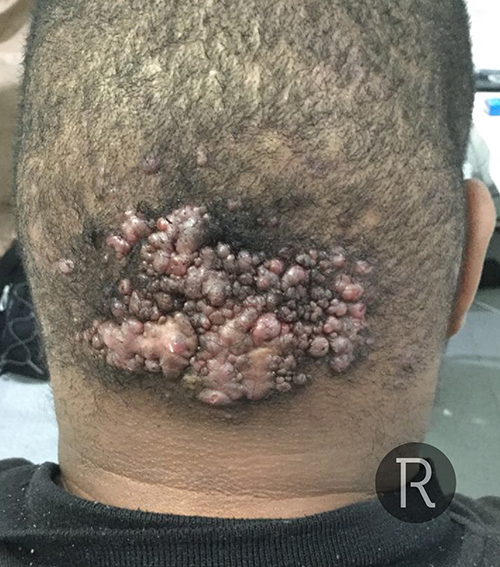






















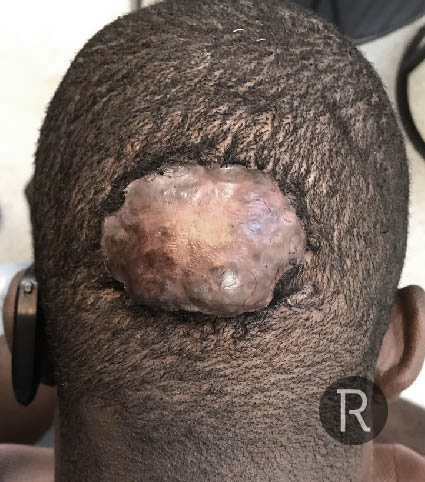


©Individual results may vary.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.

Flexible payment options for surgical treatment – 0% APR available. Spread the cost of your treatment today!
Terms and Conditions apply. *Acceptance subject to credit status.
Post-operative Scalp Keloids
Keloids can develop following surgery to the scalp. Typical surgical procedures that can result in the development of keloids, especially in ethnic backgrounds with darker skin types, include surgery for lipomas and sebaceous cysts, as well as following the repair of traumatic cuts, and even after FUE and FUT Hair Transplant surgery. Recurrence after surgical excision of keloid scars on the scalp including keloid tumours due to acne keloidalis nuchae can also occur and is particularly common in cases where patients have not received follow-up preventative treatment with YAG laser and intralesional steroid injections. This is particularly the case with those who have had surgery on the NHS due to lack of follow up.
Treatment options are dependent upon the size of the Keloid. Non-surgical treatment options include YAG laser, intralesional steroid and chemotherapy injections (5-FU). In some cases, revision surgery may be necessary. The rate of keloid recurrence in revision surgery is significant. However, follow up with nonsurgical treatments, including YAG laser and steroid injections can significantly reduce this recurrence rate. In addition, the use of silicon gel massage can also help reduce recurrence rates. At Rejuvence, we can assess the nature and state of your keloid scars and put together a bespoke treatment package that will include follow-up treatment, such as YAG laser and/or steroid injections.
Due to the stresses and strains on the NHS, keloid treatments are rarely referred to dermatologist. They are considered cosmetic concerns and hence most patients are advised by the GP to look into private alternatives. For Acne Keloidalis Nuchae, patients are often started on a combination of steroid and antibiotic cream to be applied topically. This is as per NICE guidelines but often does not yield any results. Very limited advice is also given regarding preventative measures that should be taken alongside pre-emptive, steroid and laser treatment.
At Rejuvence Clinic we have had many patients attend informing us that their dermatologists have started them on oral retinoid tablets. These medications can only be prescribed by dermatologists and are often used for the treatment of severe acne affecting the face and back. They also require careful monitoring with regular blood tests. For regular facial and back acne oral retinoid treatment can be fantastic. However, in the case of acne keloidalis nuchae oral retinoid treatment has been associated with significant worsening of keloids and they can actually grow even faster. This has been reported in the medical literature as well. We advise all our clients against oral retinoid treatment if they are suffering with Acne Keloidalis Nuchae and even if they have a history of developing acne associated keloids elsewhere on their body.
In Clinic we get this question asked a lot. Many clients ask whether a dirty or infected blade has resulted in their shaving bumps. We cannot comment on the practice of any specific barbers. However, shaving bumps are normally the result of ingrown hairs that have developed due to skin fades that are carried out using blades. Cutting against the ‘grain’ of the hair, especially if your hair is extremely curly, and you are Asian, or Afro-Caribbean, can increase the risk of developing ingrown hairs. The resulting folliculitis is usually due to infection developing due to ingrown hairs and not due to an infected or dirty blade.